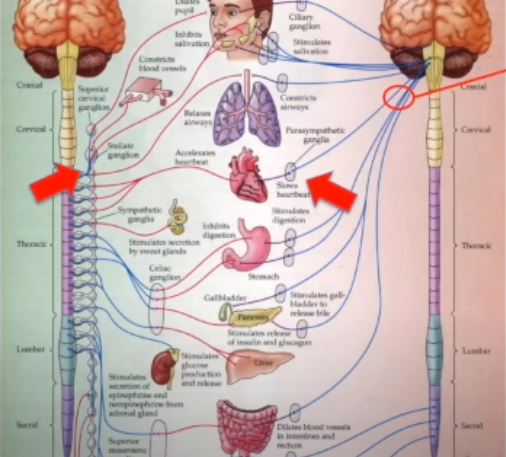
In the rare condition known as autoimmune autonomic ganglionopathy (AAG), the immune system unintentionally targets the autonomic nervous system, resulting in a series of symptoms that can greatly interfere with day-to-day functioning. Think of the autonomic nervous system as the body’s GPS, controlling vital processes like digestion, blood pressure, and heart rate without conscious control. This autopilot breaks down in AAG, resulting in a variety of erratic symptoms.
Orthostatic hypotension, a condition in which blood pressure drops precipitously when standing, is common in patients with AAG and can cause lightheadedness or fainting. As a result of the digestive system’s impaired regulation, digestive problems like extreme constipation, diarrhea, or abdominal pain are also frequent. The disease‘s widespread effects are further highlighted by the fact that many people report dry mouth and eyes, urine retention, and abnormal pupil responses.
| Attribute | Details |
|---|---|
| Disease Name | Autoimmune Autonomic Ganglionopathy (AAG) |
| Disease Type | Rare Autoimmune Neurological Disorder |
| Primary System Affected | Autonomic Nervous System |
| Main Symptoms | Orthostatic hypotension, gastrointestinal dysmotility, dry eyes and mouth, urinary retention, dilated pupils |
| Cause | Immune system attacking ganglionic acetylcholine receptors (gAChR) |
| Diagnostic Methods | gAChR antibody blood test, autonomic function tests, tilt table test, QSART |
| Treatment Options | IVIG, plasmapheresis, corticosteroids, immunosuppressants |
| Prognosis | Variable; some recover partially or fully, others require long-term symptom management |
| First Described | 1974 (as “pure pandysautonomia”) |
| Relevant Organization | Cleveland Clinic |
Because AAG is uncommon and its symptoms can overlap with those of other conditions, diagnosing it can be difficult. In order to identify antibodies against ganglionic acetylcholine receptors (gAChR), which are frequently found in AAG patients, blood tests are often part of thorough evaluations performed by healthcare professionals. Autonomic function tests, like the tilt table test, help with diagnosis by evaluating how the body’s cardiovascular system reacts to changes in position.
Immunomodulatory therapies are at the forefront of the evolving treatment strategies for AAG. By eliminating dangerous antibodies from the bloodstream, plasma exchange (plasmapheresis) relieves symptoms. The body receives vital antibodies through intravenous immunoglobulin (IVIG) therapy, which helps to regulate immune responses. The goal of immunosuppressive drugs, such as rituximab and corticosteroids, is to lessen the immune system’s assault on the autonomic nervous system.
These treatments are effective, according to recent studies. For example, studies show that although patients may benefit from IVIG or plasma exchange as first treatments, they frequently need more immunosuppressive care to maintain their improvement. This emphasizes the necessity of individualized treatment programs based on the particular presentation and reaction of every patient.
Personal accounts illuminate the human side of AAG. The difficulties faced by people with AAG are exemplified by Erica’s journey, which was shared via Dysautonomia International. She received a diagnosis of AAG following a battery of tests and consultations, and was treated with IVIG and steroids. Despite obstacles such as aseptic meningitis, Erica was able to recover from the disease and resume aspects of her life through plasma exchange.
The story of Annie Holland, a young woman from Adelaide, Australia, is another moving one. Annie was diagnosed with AAG at the age of 18, and she has been dependent on intravenous nutrition for the past ten years due to her inability to eat. Her experience demonstrates the profound effects AAG can have on day-to-day functioning and the tenacity of individuals impacted.
These tales highlight the value of prompt diagnosis and all-encompassing care. In order to comprehend AAG better and create more potent treatments, they also emphasize the necessity of greater awareness and funding for research.
The medical community is still investigating novel treatments. Novel immunosuppressive agents are one example of an emerging treatment that shows promise for patients who are not responding to conventional therapies. In order to improve the quality of life for people with AAG, ongoing research attempts to improve these strategies.
A multidisciplinary approach is necessary to manage the complex symptomatology of AAG, involving neurologists, immunologists, and other specialists. For individuals impacted, support networks and patient advocacy organizations are essential in offering community and resources, encouraging camaraderie and a sense of shared experience.
In conclusion, improvements in diagnosis and treatment provide hope even though Autoimmune Autonomic Ganglionopathy poses many difficulties. People with AAG can travel their paths with hope and resilience thanks to ongoing research, individualized medical treatment, and encouraging communities.
